BIOGRAPHY
Jordan Fuzi is a 4th Year Medical Student at the University of Newcastle, Australia. He authored this submission with his colleague, Michael Ryan, during their attachment to the Diabetes & Endocrinology Department at John Hunter Hospital. Jordan intends to pursue Physician Training on completion of his medical degree. ABSTRACT Bedside Testing for Autonomic Neuropathy: a Case Report Jordan Fuzi,*1,2 Michael Ryan,*1,3 Joyce Lim,4 David Baker,5 Georgette Goode, 6 and Katie Wynne1,2 *Equal first authors 1Department
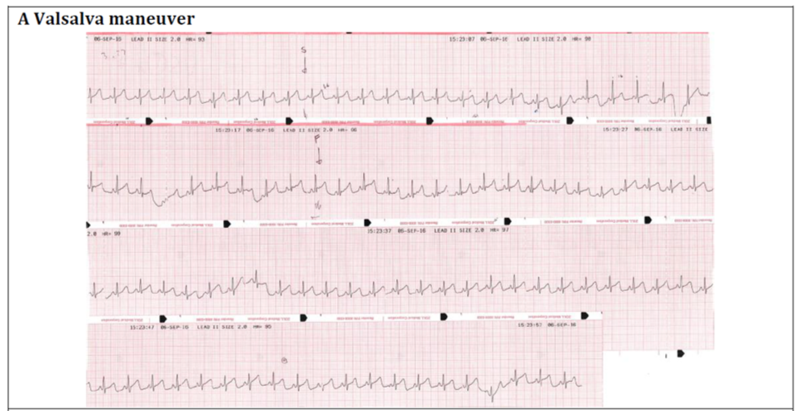
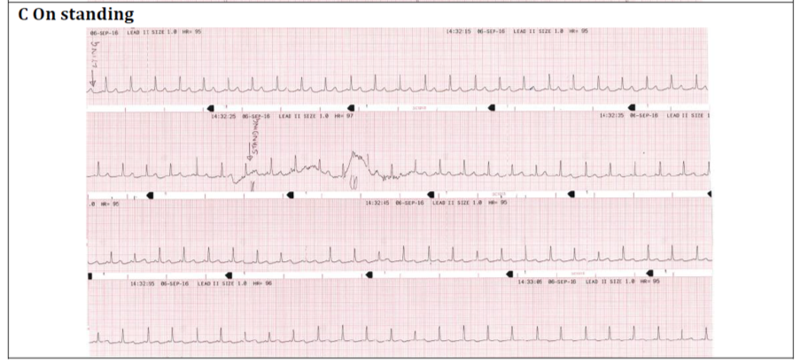
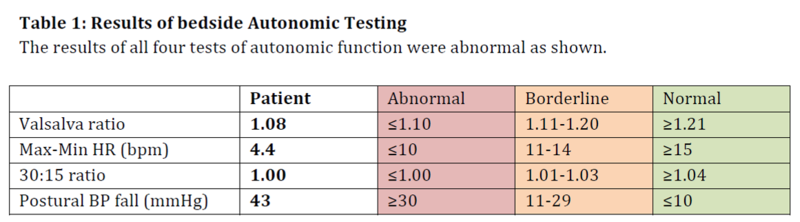
of Diabetes, John Hunter Hospital, NSW, Australia A 46-year-old woman presented with worsening nausea and orthostatic dizziness. She had type 2 diabetes diagnosed 17 years ago. Her medication included basal-bolus insulin and metformin. Insulin had been commenced three months earlier during admission for recurrent pyelonephritis. She had been prescribed metformin monotherapy despite persistent HbA1c levels >10% over several years. She had peripheral neuropathy, microalbuminuria and treated proliferative retinopathy. On standing her blood pressure (BP) fell by 35mmHg without compensatory increase in heart rate (HR). Her morning cortisol level was adequate (440nmol/l). She was investigated for autonomic neuropathy (AN). Bedside testing of BP and HR variability is an objective and reproducible method of assessing autonomic function. Figure 1 demonstrates the ECG recordings during Valsalva maneuver, deep breathing and on standing in this patient. Table 1 shows the methodology, reference ranges and abnormal results for the tests of parasympathetic (PS) function and significant postural drop that confirmed sympathetic dysfunction. The combination of orthostatic hypotension and loss of HR variability is consistent with advanced cardiac autonomic neuropathy. The patient was commenced on fludrocortisone 200mcg/day with initial symptomatic response, but has subsequently required compression stockings, sodium chloride, midodrine and caffeine tablets. Pyelonephritis as a consequence of bladder dysfunction (85 ml post-void residual) and nausea due to gastroparesis were likely additional consequences of her AN. She re-presented one month later with thoracic back pain and severe allodynia of the abdomen and lower limbs. She was diagnosed with a small-fibre variant of Guillain-Barré syndrome and ongoing AN due to chronic hyperglycaemic damage. AN should be identified early to allow intervention with improved glycaemic control. It is essential to modify cardiovascular risk factors as increased mortality may occur as a consequence of silent myocardial ischaemia, coronary artery disease and stroke. Physicians can test for AN with the use of simple, non-invasive, standardised bedside test. Figure 1: ECG monitoring from lead II A. HR response to a Valsalva maneuver performed by
forced expiration into a sphygmomanometer sufficient to maintain a pressure of
40mmHg for 15 seconds.
Valsalva ratio is calculated as the ratio of the shortest R-R interval during the maneuver and the longest R-R interval after; in normal physiology this should result in a reduction in HR mediated by the PS nervous system. Max-Min HR is calculated as the mean difference between the maximum and minimum HR in 6 deep breathing cycles (inspiration/expiration). The longest and shortest R-R interval is measured for each cycle and then converted to beats/minute (1500/R-R mm); a lack of HR variability has 80% specificity for PS dysfunction. The 30:15 ratio is calculated as the ratio of the longest R-R interval at the 30th beat to the shortest interval at the 15th beat after standing, if the PS system is intact this should result in variability and therefore a longer ratio. A postural fall in systolic BP is calculated by subtracting the lying measurement from that taken two minutes after standing; in normal physiology BP should be maintained by sympathetic control of vasoconstriction. |