
ABSTRACT Prevalence Of Medication Non Adherence In patients With Acute Coronary Syndrome In A Tertiary Care Hospital - National Hospital Of Colombo, Sri Lanka (NHSL)
1Fernando B K N, 2 Tissera W A J N, 1Hancock N, 3Rodrigo E S S, 4Jayamanne B D W, 4Wickramasinghe W M H G S B.
1Department of General Medicine, Royal Hobart Hospital, Tasmania. 2National Hospital of Colombo Sri Lanka. 3Royal Hobart Hospital, Tasmania. 4Ministry of Health, Colombo, Sri Lanka.
Abstract
Background
Medication Non adherence (MNA) is very common around the world. The estimated prevalence is 45-55% (Norman SA et al, Amaral P). The burden is huge to the country health care system especially when the health is free.
Aims
The main aim was to evaluate the prevalence MNA at NHSL. The other objectives were to assess the reasons for MNA, to assess factors associated with MNA and to assess major contributory factors for MNA.
Methods
This was a descriptive cross sectional study at NHSL from 1 January 2013, involving 384 in ward medical patients. Patients with previous ischaemic heart disease (IHD) and cardiovascular co-morbidities admitted to 16 General Medical Wards, in whom the diagnosis of ACS was made were included. Sample size was calculated using the formula by Lwanga & Lemeshow (1991). MNA was assessed using Morisky Medication Adherence Scale (MMAS).
Results
Amongst 384 patients, 53.1% were female. 59.1 Percent of patients were found to have MNA ranging from mild, moderate to severe according to MMAS. A Majority (56.4%) had moderate MNA. Forgetfulness and /or negligence were commonly reported- 85 (22.2%). Improvement of disease symptoms, false perception that the drug is not needed, cost of the drugs and fear of drug side effects were the other causes of MNA ranked 2nd to 5th. Multivariate logistic analysis demonstrated a significanet association between lower level of education and MNA. Univariate logistic regression analysis failed to demonstrate a significant association between MNA and gender, ethnicity, marital status, level of education, area of residence, age, alcohol consumption, smoking behaviour.
Conclusion
Prevalence of MNA is high at 59.1% in the largest tertiary care hospital in Sri Lanka in patients with ACS. Measures needs to be implemented to address the main reasons for MNA. A system has to be in place to remind the patients to take their medications. Improving the awareness of usefulness of medication, proper education regarding medication side effects is mandatory too. Reducing the cost of drugs will also reduce MNA.
Mysterious Abdominal Pain And Disseminated Intravascular Coagulation In A 60 Year Old - Disseminated Hepatic Angiosarcoma
Authors: 1Fernando B K N, 1Butcherine K 2 Harle R A, 3Ritchey D M Affiliation: 1Department of General Medicine, Royal Hobart Hospital, Tasmania. 2 Department of Radiology, Royal Hobart Hospital, Tasmania, 3 Department of Forensic Pathology, Royal Hobart Hospital, Tasmania
Abstract Text:
Introduction
Angiosarcoma is a rare high-grade malignant vascular neoplasm [1]. It is the most common sarcoma of the liver [2]. It occurs in older patients (>60 years) and more commonly in men. Presentation is with generalized, nonspecific symptoms such as weight loss, fatigue, abdominal pain and rarely with coagulopathies [3]. Our patient presented with undifferentiated abdominal pain, disseminated intravascular coagulopathy (DIC) and haemolytic anaemia (HA).
Case Report
A 60 -year-old morbidly obese man (BMI-52kgm2) was admitted with generalized abdominal pain, weight loss of 50kg over 6 months and 12 months of maleana. His comorbidities were Type II diabetes, onychomycosis and gastro-oesophageal reflux. Longstanding medications were, Griseofulvin, Lantus, Metformin, Rabeprazole and Rosuvastatin. Truncal purpura, jaundice and nonspecific abdominal pain were noted, as was a family history of bowel and breast cancer.
Investigations revealed chronic DIC and DAT negative haemolytic anaemia. Abdominal CT showed constipation.
He represented after 2 weeks with worsening abdominal pain, jaundice and delirium. Abdominal imaging remained unhelpful as did a full body PET scan.
Over 72 hours he developed multiorgan failure and worsening coagulopathy. His condition deteriorated rapidly despite cardiopulmonary support and the decision was made with his family to provide comfort care.
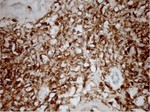
At autopsy the liver was cirrhotic with multiple haemorrhages. Microscopy showed an infiltrative malignancy with strong positive staining for an endothelial stain , CD-31, indicative of hepatic angiosarcoma.
Figure 1- Liver at autopsy Figure 2-CD31 positive immunological stain
  Discussion
Hepatic angiosarcoma has a very poor prognosis with an average survival of 6 months, even when less dissemination, multi-organ failure and DIC are evident at presentation. Diagnosis is often post-mortem and no single treatment regimen has been established. Palliative chemotherapy is occasionally indicated for symptom control.
References
1. Suriawinata AA et al. Malignant liver tumors. Clin Liver Dis 2002; 6:527.
2. Bioulac-Sage P, et al. Benign and malignant vascular tumours of the liver in adults. Semin Liver Dis 2008; 28:302.
3. Locker GY et al. The clinical features of hepatic angiosarcoma: a report of four cases and a review of the English literature. Medicine (Baltimore)1979;58(1):48–64.
Title: Neck Of Femur Patient Management Standards In Royal Hobart Hospital Tasmania Background: Neck of Femur (NOF) fractures are a commonly encountered clinical problem among elderly patients and are a significant burden on the Australian healthcare system [1]. Aims: The main aim of this audit was to evaluate whether Royal Hobart Hospital (RHH), meets the established National standards of care for the management of NOF fractures by undertaking surgery within 48 hours [2]. Other objectives were to assess length of stay and assess in hospital post-operative mortality, and understand discharge destination after surgery. These outcomes are compared to three similar Australian studies from hospitals with specialist orthopaedic units [Liu et al, Chia et al, NOffRA]. Methods: This audit was on patients admitted to RHH, with NOF fractures over a period of one year. Excluded from the study were patients who had multi-trauma-related fractures, in hospital NOF fractures, and in whom non-operative management strategy was undertaken. Descriptive statistics and meta-analysis were performed. Results: Overall, amongst 126 patients with NOF fractures admitted to RHH from 1 September 2014 to 31 August 2015, 105 met inclusion criteria. 67.6 Percent were female. Mean age 81.6 years. Most (29%) were in the 80-85 year age group. A total of 88.57 % of patients were operated on within 48 hours. 62 Percent, 9.5% and 17.1% were operated <24hours, within 24-36 and within 36 - 48 hours respectively. Mean length of stay (LOS) was 14.2 days and in-hospital post operative mortality was 10.5 %. Seventy-two patients were from home and 29.4% discharged to a rehabilitation unit. All patients from nursing homes (NH) were discharged back to NH. Conclusion: This audit suggests that RHH serviced by Orthopaedic surgeons meets the established standards of care for management of most NOF fractures in terms of time to surgery ( verses 67–86 %). The prolonged LOS of 14.2 days (verses 7.7–13.7 days) with only 29.4% (versus 67% - 83.2%) discharged to a rehabilitation unit may reflect the limited access to rehabilitation in a timely fashion. The mortality of 10.5% (versus 2–7 %) was observed in patients aged >84 years. Considering all these observations, it is worthwhile to explore the best model of care managing NOF fracture patients. Sending post-operative patients to a rehabilitation unit in a timely manner will likely reduce the number in patient days in an acute care hospital. References: Sanders KM et al. Health burden of hip and other fractures in Australia beyond 2000. Projections based on the Geelong Osteoporosis Study. Medical Journal of Australia. 1999; 170: 467-470. Mak JCS et al. Evidence-based guidelines for the management of hip fractures in older persons: an update. Medical Journal of Australia 2010; 192 (1): 37-41 |