
BIOGRAPHY
Rhys is an Intern at The Wollongong Hospital, NSW Australia. He previously worked as an ICU respiratory physiotherapist before and during medical school. He underwent multiple medical students rotations in rural areas of NSW including Nowra, Lismore and Broken Hill. Rhys has a passion for regional/rural medicine and is interested in becoming a general physician. ABSTRACT
Stroke in a young man with a murmur: A Case Report
Gray R
Introduction: This case report describes a 40 year-old male who presented with symptoms consistent with a large middle cerebral artery stroke. The report illustrates the causes of stroke in a young person, and the pathogenesis of stroke due to rheumatic heart disease. It also highlights the complication of cytotoxic cerebral oedema that can occur after a large stroke. The use of intravenous thrombolysis and mechanical thrombectomy in the treatment of stroke is also discussed and compared.
Case description: A fit 40 year old male collapsed at home and was brought to hospital by ambulance. On examination he was confused with a left hemiparesis and dysarthria. A Computerized tomography (CT) scan of his brain showed no signs of haemorrhagic stroke. The patient was thrombolysed within 4 hours of symptom onset. He then deteriorated and a subsequent CT brain scan showed development of cerebral oedema, which was managed by decompressive hemicraniectomy. On examination in ICU post hemicraniectomy, a diastolic murmur with an opening snap was identified and an echocardiogram showed tight mitral stenosis with a large dilated left atrium. These findings were consistent with rheumatic heart disease. The patient was anticoagulated with warfarin, commenced on penicillin intramuscular injections and was discharged to a rehabilitation hospital with cardiology follow up for a possible percutaneous balloon mitral valvuloplasty.
Discussion: In this case report the patient’s thrombus was hypothesized to have been caused by intermittent atrial fibrilation due to rheumatic mitral stenosis. Decompressive hemicraniectomy is a surgical procedure used to reduce the intracranial pressure caused by cytotoxic cerebral oedema. Five large randomized control trials [1-5] found that intra-arterial thrombectomy is superior to standard treatment with intravenous thrombolysis alone for a large, proximal, anterior artery occlusion. The widespread clinical use of mechanical thrombectomy is often restricted to major stroke centres that have the resources and personnel available.
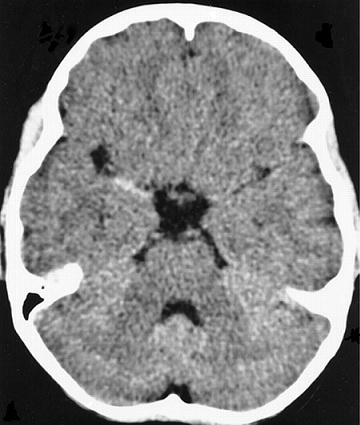 Figure 1: Preoperative CT scan demonstrating a positive hyperdense middle cerebral artery sign in the right main stem.
References
1. Berkhemer O, Fransen P, Beumer D. A randomized trial of intraarterial treatment for acute ischemic stroke. New England Journal of Medicine. 2015; 372:11.
2. Goyal M, Demchuk A, Menon B. Randomized assessment of rapid endovascular treatment of ischemic stroke. New England Journal of Medicine. 2015; 372:1019.
3. Saver J, Goyal M, Bonafe A. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. New England Journal of Medicine. 2015; 372:2285.
4. Campbell B, Mitchell P, Kleinig T. Endovascular therapy for ischemic stroke with perfusion-imaging selection. New England Journal of Medicine. 2015; 372:1009.
5. Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015; 372:2296.
Importance of clinical features and risk factors in the assessment of pulmonary embolism in a rural hospital: A Clinical audit.
Gray, R
Aim:
This study was carried out to establish the demographics, clinical features and risk factors of all the patients that developed a pulmonary embolism (PE) at Lismore Base hospital (LBH) over a 12 month period.
Method:
A retrospective case record review of 65 patients with a diagnosis of pulmonary embolism was carried out at Lismore base hospital for the period between June 2013 and July 2014. 6 patients were excluded from the study as they were incorrectly coded by medical records and did not have a PE during their admission. A database with relevant demographic information, clinical presentation, risk factors and diagnostic modalities was developed with information from patient notes and medical records.
Results:
The age of patients who developed a PE ranged from 28-89 years of age. The mean age was 63.47, the median age was 63. 53% of patients were female and 47% were male.
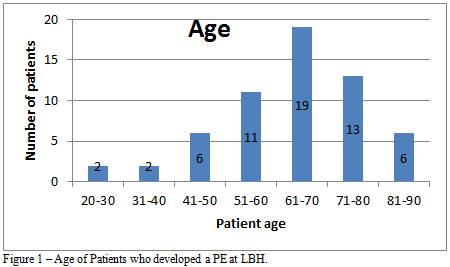 The most common presentations were shortness of breath (69%), chest pain (53%) and calf pain or swelling (12%). Only 7% of patients had no reported symptoms.
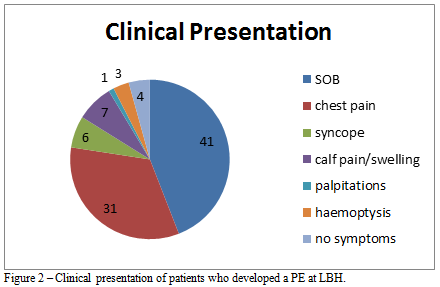 The most common risk factors identified were current or past history of smoking (53%), active cancer (36%), past history of DVT or PE (32%), recent immobility (27%) and surgery in the last 3 months (15%). Only 12% of patients did not have any identifiable risk factors for developing a PE. 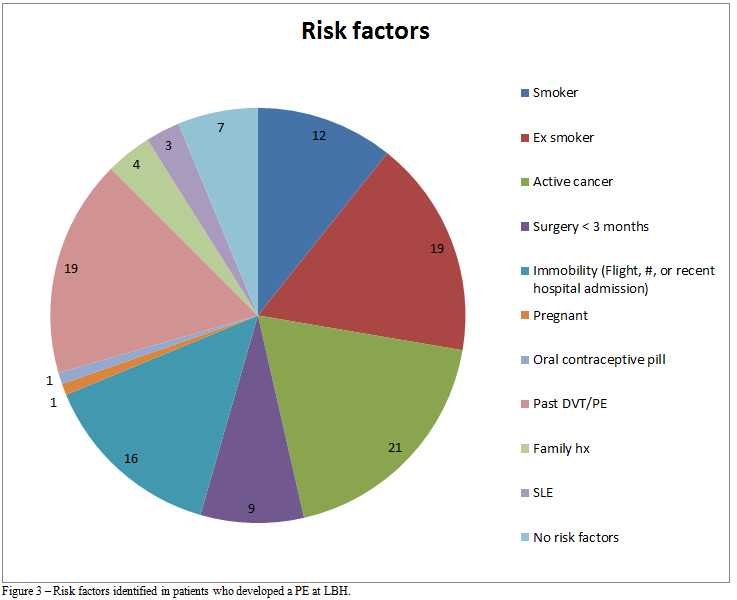 88% of patients reviewed had a venous ultrasound during their admission. A deep vein thrombosis was found in 50% of the patients who had an ultrasound. 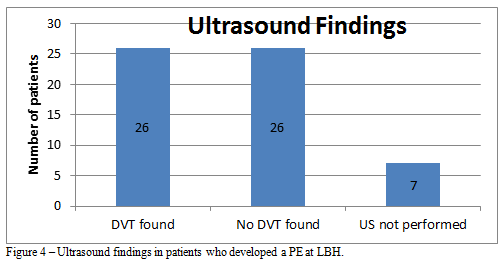 Conclusion:
Useful information to help identify acute PE is based upon characteristics of the history, physical examination, and venous ultrasound. In the patients that were found to have an acute pulmonary embolism, only a small percentage did not have a number of risk factors or important clinical manifestations suggestive of PE. Clinical assessment is useful for the identification of patients in whom further examination is required.
|